Learn More about Our Partnership with a Lead Researcher at John’s Hopkins School of Medicine
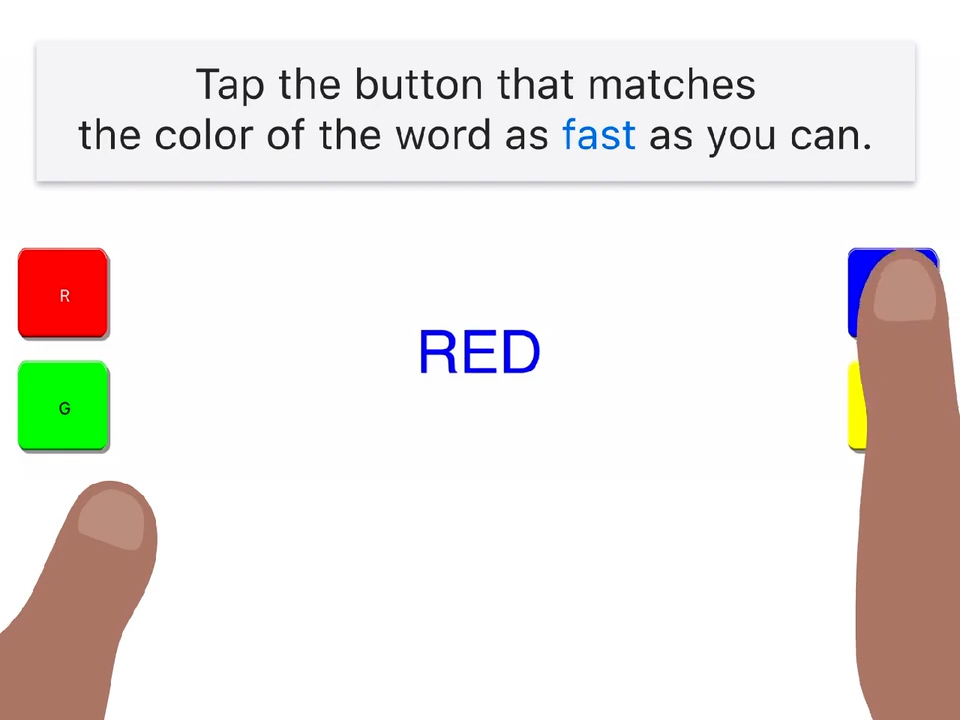
December 1st is World AIDS Day. To bring light to the great work being done to advance HIV/AIDS research, we are highlighting BRACE (BrainBaseline Assessment of Cognition & Everyday Functioning), our technology that assesses cognition in people living with HIV.
The Clinical ink team has long had a collaborative relationship with Dr. Leah Rubin from Johns Hopkins University School of Medicine. Since 2018, we have equipped her HIV research with BRACE for use in-clinic.
Dr. Rubin is an Associate Professor of Neurology, Psychiatry, and Epidemiology and focuses on researching at-risk individuals’ cognitive and mental health. She uses big data sets to find patterns and predictors for that population, and then drills down to identify the mechanisms behind cognitive or mental decline. With a focus on people with HIV, Dr. Rubin’s work has been a part of the National Institute of Health’s Women’s Interagency HIV Study (WIHS) and Multicenter AIDS Cohort Study (MACS).
Adapting Cognitive Tests for In-Clinic Administration
Most HIV clinic visits focus on antiretroviral medication adherence, leaving patients’ cognitive and mental health forgotten. Traditionally, cognitive testing also requires a great deal of training on the part of a test administrator; even those well-trained may differ and deliver data inconsistencies. Because Clinical ink’s cognitive assessment for HIV positive people is self-administered, they remove the burden of training a test administrator AND deliver more consistent data.
Dr. Rubin says, “Being able to hand an iPad over and have [patients] complete the BRACE cognitive battery, basically [takes] away all of the burden.”
In collaboration with Dr. Rubin, the advanced technology team at Clinical ink team adapted the HAND in Hand at home iPhone app to BRACE, an in-clinic iPad app for Dr. Rubin to deploy at the John G. Bartlett HIV Practice of Johns Hopkins Hospital in Baltimore, Maryland.
“We needed some sort of electronic method that can be implemented within these busy clinics,” said Dr. Rubin. “When patients are waiting, you have 10 minutes. We can incorporate this into the busy routine of clinic care.”
Study goals
The primary goal for this study was to assess as many people as possible to understand the cognitive burden of people with HIV, and then link that cognitive data to patient medical records. Additionally, there was a desire to study the stability of cognitive function in people with HIV, because it seems to fluctuate. Because most cognitive testing is typically done at infrequent intervals, it does not allow for clear visualization of fluctuation; however, BrainBaseline’s application allows for quick, low-cost, and more frequent testing.
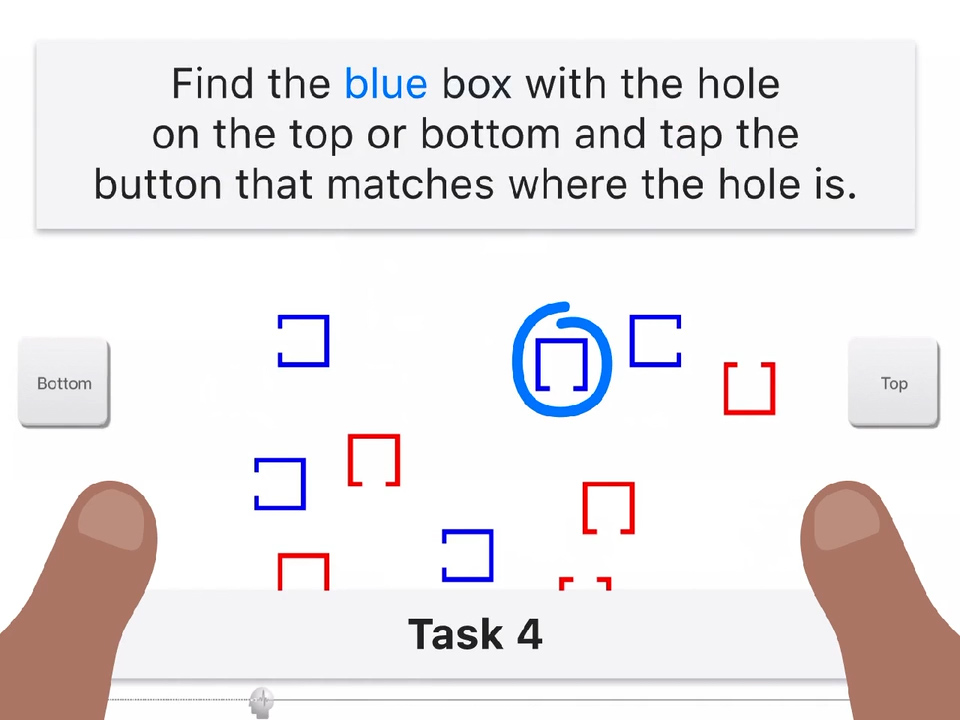
Dr. Rubin intended the initial BRACE protocol as a short screening tool that can flag individuals’ area of cognitive impairment. After patients are flagged, more in-depth testing can be done.
“BRACE is a nice screener for minor forms of cognitive impairment which are hard to pick up on.”
Then, Now, and Next Steps
In 2019, Dr. Rubin envisioned the BRACE data set growing into the thousands—and indeed, now in December 2022, the numbers stand at over 2,275 people enrolled. Because these cognitive assessments are more widely used in HIV clinics, cognitive decline can be better identified and quantified, which can in turn lead to the identification of underlying problems. For instance: Is HIV causing this cognitive decline, or is it the medication? Is it both? Identifying impairment can also allow for more customized treatments.
“For me it’s just about getting BRACE out there,” said Dr. Rubin. “The data will convince people. If the tool is good, the data is good … [the Clinical ink team] has developed an exceptional product.”
With mobile apps for both Apple and Android phones, at-home testing can be completed by a larger population, allowing the BRACE data set to continue to grow. We look forward to partnering to make Dr. Rubin’s vision a reality.
“[This is] the tip of the iceberg,” said Dr. Rubin. “So many amazing things that will spin off of this.”
Interviewee
Dr. Leah Rubin, Ph.D., M.A., M.P.H.
Associate Professor of Neurology,
Johns Hopkins University School of Medicine
